The mandible is the only movable bone of the facial skeleton, as the condyle portion articulates with the temporal bone to form the temporomandibular joint (TMJ). A myriad of benign and malignant lesions (Tumours/Pseudotumours) may affect the TMJ, and many remain undiagnosed until they become symptomatic or are incidentally discovered through imaging. Further complicating diagnosis is the fact that these lesions occur relatively rarely, can present with clinical manifestations similar to more common TMJ dysfunction (TMD), and with radiological findings in some lesions that may be non-specific. This difficulty can easily lead to misdiagnosis and delay in treatment, which can increase patient morbidity and in the case of malignant tumours, patient mortality.
Certain clinical manifestations can help the clinician distinguish between TMD and tumor disease affecting the TMJ. They include numbness in regions innervated by trigeminal nerve branches, hearing loss, constant pain not influenced by mandibular movement, progressively increasing severity of symptoms, progressive facial asymmetry, a lack of response to conservative treatment, malocclusion, the presence of swelling (including adenopathies), unexplained weight loss, ear suppuration or swallowing difficulties. Occlusal alterations, along with pre-auricular swelling, were the most suggestive signs for tumors affecting the TMJ.
Tumor presentation may be intrinsic (within) or extrinsic (adjacent) to the temporomandibular joint. Intrinsic tumors can develop within the condyle, temporal bone or coronoid process, while extrinsic tumors may affect the morphology of structures and TMJ function without directly invading the joint. For example, synovial chondromatosis, is rare, intra-articular or intrinsic tumor, corresponding to the metaplastic transformation of synovial tissue into chondroid tissue.
A review of the literature found that the average time from onset of symptoms to consultation and treatment was 2.5-3 years for benign lesions, and 1 year for malignant lesions. Although these lesions are rare, it is imperative to understand the clinical, radiological, and histological presentation in order to provide an accurate diagnosis and timely treatment plan. The clinician should recognize that if conservative treatment measures for TMD fail or symptoms progress, that referral for additional advanced diagnostic imaging and specialist consultation may be required.
Case Report
A 68-year-old male presented in September of 2017 on referral from his physician regarding a TMJ associated mass. He had originally seen his physician regarding a complaint of right orbital pain. The patient was sent for MRI and CT imaging, which showed no ophthalmologic abnormalities. However, it incidentally discovered a large radio-opaque mass in the right TMJ region with extension into the middle cranial fossa. The radiographic diagnosis provided was synovial osteochondromatosis.
Patient symptoms were relatively mild with occasional, mild discomfort affecting the right TMJ region.
The medical history revealed prior treatment for glaucoma and hypertension.
Fig. 1A
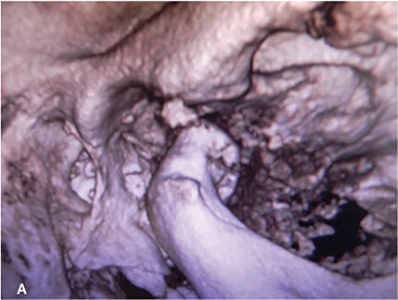
Fig. 1B

Fig. 2A, 2B
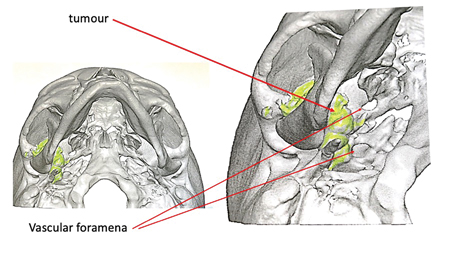
Fig. 3A

Fig. 3B

Fig. 4A
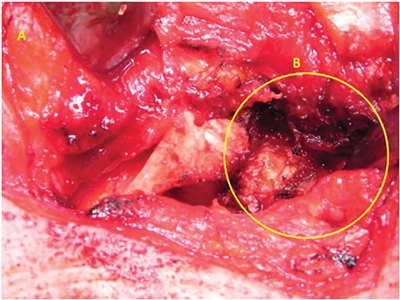
Fig. 4B
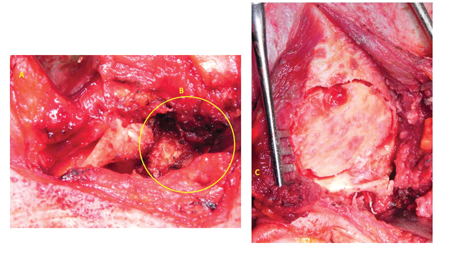
Fig. 5A
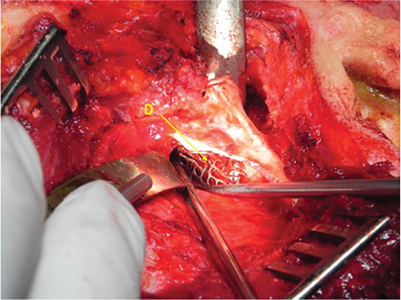
Fig. 5B
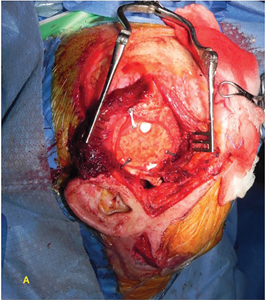
Fig. 6A

condyle repositioned and stabilized with miniplates.
Fig. 6B

condyle repositioned and stabilized with miniplates.
Fig. 7A

Fig. 7B

Clinical examination revealed a normo-cephalic male with normal eyes, ears, nose and throat. There was mild asymmetry of the mandible with very mild chin deviation to the left and an orthognathic profile. The muscles of mastication exhibited no pain to palpation. He had mild discomfort of the right TMJ with firm palpation. Mouth opening was adequate but limited to 35 millimeters, with slight deviation to the right.
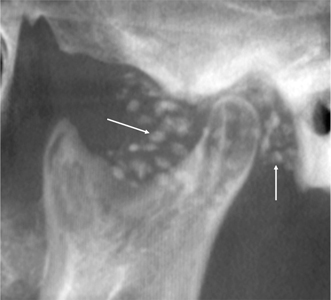
The panoramic x-ray displayed a mildly hyperplastic right TMJ, and radiopaque, circular densities were noted surrounding and extending anterior to the condylar head.
A cone beam CT scan (CBCT) was acquired and illustrated a large, radiopaque mass wrapped around the right condylar head and filling the glenoid fossa, extending along the skull base to the foramen ovale and foramen spinosum, with areas of erosion into the middle cranial fossa.
This presentation was consistent with a diagnosis of ‘synovial osteochondromatosis with intra-cranial extension’. Presurgical neurosurgery and neuroradiology consultations were obtained. A collaborative treatment plan for surgical excision was formulated with presurgical embolization of the right intermaxillary artery, middle meningeal artery and accessory meningeal artery in the hopes of avoiding severe intra-operative bleeding. A preoperative CT angiogram showed close approximation of portions of the tumour to the internal carotid artery.
In December 2017, the patient was taken to the operating room where in collaboration with both oral and maxillofacial surgery and neurosurgery, the surgery was carried out under general anaesthesia The surgery was performed using surgical navigation, a technology where a probe placed into different parts of the wound to help localize, in real time on a 3D CT, the proximity to other vital structures like large arteries.
The surgical approach involved the elevation of a right sided hemi-coronal flap, exposing the temporal bone, zygomatic arch and TMJ region. A retromandibular incision was also performed, exposing the mandibular ramus, sigmoid notch and condyle. Bone plates were adapted to the form of the mandible and then set aside. Osteotomies were performed, and the condyle and coronoid process removed to provide surgical access. A zygomatic arch osteotomy was also carried out to further facilitate access to the skull base. Examination of the temporomandibular joint showed complete destruction of the articular disc. The tumour was seen to encircle the condyle and extend anteriorly to the base of skull. A perforation in the glenoid fossa was noted. At this point, neurosurgery performed a craniotomy in order to access the middle cranial fossa. The intracranial portion of the tumour was defined and removed, followed by the removal of the extracranial portion of the tumour. The external sheath of the carotid artery was fully visualized upon completion of the tumour removal. Neurosurgery repaired the cranial base perforation from within using titanium mesh. The bone flap was then replaced and stabilized with three fixation bone plates. A temporalis fascia graft was harvested from the exposed temporalis muscle and used to construct a new disc by suturing to the posterior, medial and anterior aspects of the joint space. The TMJ condyle was then replaced and rigidly fixated with the previously adapted bone fixation plates. The zygomatic arch was also replaced and fixated with the prepared bone plate. Closure was routine and performed in tissue layers. Dental arch bars placed during the procedure were used to guide the patient’s occlusion using dental elastics. A pressure bandage was applied intra-operatively and the patient taken to the neurosurgery intensive care unit in a favourable and stable condition. The hospital stay was uneventful.
Fig. 8

Fig. 9

Fig. 10
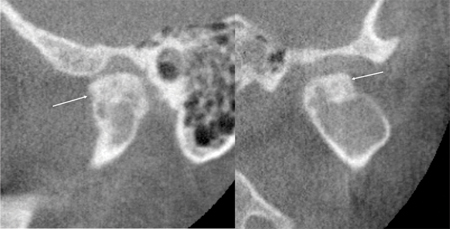
Fig. 11

Fig. 12
Postoperatively, the patient had anticipated swelling and bruising. There was some pain, which resolved quickly. There was transient weakness of the right temporal branch of the facial nerve, which resolved over subsequent months. The patient was seen regularly throughout the first year with progressive, ongoing improvement. The occlusion was stable with improved range of motion. Neurosurgery follow up was also favourable. A postoperative CT scan acquired months post operatively showed no presence of tumour.
At the one year follow up examination there was no pain, normal mandibular range of motion, a stable occlusion, and normal cranial nerve VII function.
Discussion
There is an adage often quoted in North American training programs that states that “if one hears hoof beats, one should think of a horse before a zebra”, which is a way to emphasize to the trainee that “common entities occur commonly”. The obvious truth of this statement serves to ensure that the clinician does not get distracted from the obvious, or take a tangential approach and misdiagnose an entity or condition.
This article self-admittedly deals with a group of “zebras” and serves only to prime the reader to not dismiss the subtle clues that indicate that the lesion in question does not quite fit the presentation of a common TMD entity. While the “zebra” diagnoses are uncommon, they do exist, and it is critical that the knowledgeable clinician identify and combine the subtle clinical, radiologic, and histopathological presentation in order to correctly identify and treat such pathologies. (Table 1)
Table 1

loose bodies) (A few other varieties not listed may exist) (Adapted from Perez -Maclean)
The TMJ complex is composed of bone and soft tissue structures including the temporal bone, mandibular condyle and coronoid process, articular disc, articular capsule, synovium as well as associated muscles and ligaments. The innervation of the mandibular condyle is carried by the auriculotemporal and masseteric branches of the third division of the trigeminal nerve (V3). The tumors and pseudotumors presented can develop from within or on any of these bone or soft tissue structures.
Tumours and pseudotumors may present with subtle TMD symptoms and are often asymptomatic. They can grow slowly, often attaining a considerable size before becoming clinically evident. A noticeable change in occlusion, with mandibular deviation or facial asymmetry can be hallmark signs of a condylar tumor. Similarly, the sudden onset of facial paralysis or an area of paresthesia can represent signs of both benign and malignant entities.
Malignant tumors of the TMJ are extremely rare. They may be primarily intrinsic in nature such as an osteogenic sarcoma or extrinsic such as an extension of a parotid salivary gland malignancy. They may also represent a metastatic lesion which has spread to the joint, with the most common primary carcinomas being breast, lung and prostate. Another two entities reported to be remarkably rare are multiple myeloma and malignant fibrous histiocytoma. Although the initial symptoms may be similar to TMD, malignant tumors may have increased pain, swelling, and paresthesia. A recent review of over 700 cases found that the mean age at presentation was 47 years, with an equal 1:1 sex ratio of females to males. Surgical resection and reconstruction represent the mainstay modality of treatment, coupled with radiotherapy and/or chemotherapy.
Surgery represents the most common form of treatment. An open preauricular approach to the lesion is a common surgical technique, although arthroscopic surgery is sometimes used for smaller articular loose bodies or synovial chondromatosis cases. It is not uncommon for some cases to require either immediate or delayed tissue reconstruction, depending on the specific tumor and its location and effect on surrounding structures.
Conclusion
The purpose of this paper was to provide an overview of benign and malignant lesions of the TMJ, as a significant group can occur in this region. (See figures 8-12 for examples.) The radiologic findings in many cases are non-specific. Likewise, no unique clinical manifestations exist for identifying pseudo-tumors, benign tumors, and malignant tumors. Advanced imaging in the form of CBCT, CT and MRI can be helpful in distinguishing a mass from simple TMD disorders. These aspects serve to underscore the importance of understanding both the clinical presentation and the histopathology, to determine the correct diagnosis and formulate an ideal treatment plan. Ultimately, the final diagnosis depends on intraoperative frozen section biopsy and intra/post-operative histopathology. Treatment generally involves surgery, and relapse is observed in approximately 10% of cases, particularly among the malignant tumors.
Oral Health welcomes this original article.
Acknowledgment: The authors wish to acknowledge Dr. Mathilde Sarlibous (OMFS), Dr. Eric Duncan (neurosurgery) and Dr. Walter Montanera (interventional neuroradiology) who also provided care to the patient described in the case report.
References
- L. Perez -Mclean et al. Benign and malignant lesions affecting the mandible condyle. JSM Dent 8(2) 1127, 2020.
- R. Poveda-Roda et al. Pseudotumors and tumors of the temporomandibular joint. A review. Med Oral Patol Oral Cir Bucal 18(3) e392, 2013.
- F. Yibulayin et al. Malignant tumors of the temporomandibular joint. BMC Cancer 20, 967, 2020.
- M. E. Yurttutan, et al. Benign Tumors of Temporomandibular Joint. In: Y. Emes, B. Aybar, & G. Dergin (Eds.), Temporomandibular Joint Pathology–Current Approaches and Understanding. IntechOpen. https://doi.org/10.5772/intechopen.72302, 2017
- SE Perschbacher, Temporomandibular joint abnormalities. In: White, Stuart C., and M. J. Pharoah. Oral radiology: principles and interpretation. St. Louis, Mo: Mosby/Elsevier. 2014. Pg 492.
About the Authors
 Bruce R Pynn is Oral Health’s editorial board member for oral and maxillofacial surgery. He maintains a private practice in Thunder Bay, ON. He is Chief of Dentistry, Thunder Bay Regional Health Sciences Center.
Bruce R Pynn is Oral Health’s editorial board member for oral and maxillofacial surgery. He maintains a private practice in Thunder Bay, ON. He is Chief of Dentistry, Thunder Bay Regional Health Sciences Center.
 Iain A. Nish is a graduate of The University of Toronto in both Dentistry and Oral & Maxillofacial, and completed a Fellowship in Plastic & Reconstructive Surgery in Basel, Switzerland. Dr. Nish was a Staff OMFS at Sick Kids Hospital for two decades.
Iain A. Nish is a graduate of The University of Toronto in both Dentistry and Oral & Maxillofacial, and completed a Fellowship in Plastic & Reconstructive Surgery in Basel, Switzerland. Dr. Nish was a Staff OMFS at Sick Kids Hospital for two decades.
 Susanne Perschbacher is a part-time Assistant Professor, Teaching Stream, Faculty of Dentistry, University of Toronto. She is also a consultant Oral and Maxillofacial Radiologist for Sick Kids Hospital and maintains a private Oral Radiology practice.
Susanne Perschbacher is a part-time Assistant Professor, Teaching Stream, Faculty of Dentistry, University of Toronto. She is also a consultant Oral and Maxillofacial Radiologist for Sick Kids Hospital and maintains a private Oral Radiology practice.
 Kelsey Won is a junior resident, Oral and Maxillofacial Surgery, Faculty of Dentistry, University of Toronto.
Kelsey Won is a junior resident, Oral and Maxillofacial Surgery, Faculty of Dentistry, University of Toronto.
 David J. Psutka is Assistant Professor, Oral and Maxillofacial Surgery, Faculty of Dentistry, University of Toronto, Senior Surgeon, Mount Sinai Hospital Centre of Excellence for Advanced TMJ Reconstructive Surgery, Co-director, University of Toronto Fellowship Program in Advanced TMJ and Orthognathic Surgery, Private Practice, Fountain View Oral, Facial and Implant Surgery, Mississauga.
David J. Psutka is Assistant Professor, Oral and Maxillofacial Surgery, Faculty of Dentistry, University of Toronto, Senior Surgeon, Mount Sinai Hospital Centre of Excellence for Advanced TMJ Reconstructive Surgery, Co-director, University of Toronto Fellowship Program in Advanced TMJ and Orthognathic Surgery, Private Practice, Fountain View Oral, Facial and Implant Surgery, Mississauga.









